APPENDIX C
Contents
|
|
Page |
|
Blood Analyses |
324 |
Normal values |
324 |
Preparation of precipitants |
324 |
Blood and plasma volume Modification of Gregersen method |
|
Procedure for determination of blood volume |
330 |
Blood Chemistry Nonprotein nitrogen products (Nonprotein nitrogen in plasma. creatinine in plasmauric acid in plasma urea nitrogen in plasma) |
|
Acid-base analyses (Blood pH. serum sodium. serum potassium. serum calcium. magnesium in plasma. phosphorus in plasma.CO2 combining power of plasma. chlorides in plasma. lactic acid in plasma) |
337 |
Glucose in plasma |
343 |
Sulfonamides in whole blood |
343 |
Determination of methemoglobin |
343 |
Plasma bilirubin |
344 |
Hemoglobin, hematocrit, and plasma protein |
344 |
Plasma hemoglobin determination |
344 |
|
Liver Function Test |
345 |
|
Renal Function Tests (Mannitol. para-amino hippuric acid. phenosulfonphthalein test) |
346 |
|
Urinalyses (Routine. the benzidine test. titratable acidity. organic acids. creatinine and creatine) |
349 |
|
Determination of Myoglobin (Urine and tissue) |
354 |
Biochemic Methods
The biochemic procedures to be used in this study were selected on the basis of their accuracy and their applicability to the anticipated conditions in a combat area. Many procedures were modified so that the critical quantitative readings might be made on the spectrophotometer. Those described for the determination of blood volume; plasma magnesium, serum sodium; creatinine and creatine in urine; the bromsulfale in and phenolsulfonphthale in tests, and the determination of myoglobin, for example, offer generally useful modifications of standard procedures. Methods in which any changes in the standard procedure were made are described in detail.
Blood Analyses
Normal Values in the Blood Analyses
The ranges of normal values for analyses made on the blood as shown in Table 118 are essentially those given in the literature. For convenience it was often necessary to assume a single figure as representing the standard normal level for a particular analysis in order to contrast it with the average findings in certain groupings of the cases in this study. The figure used for the standard normal was selected as a result of our experience with each method.
Preparation of Blood and Plasma Protein Precipitants
TUNGSTIC ACID FILTRATE
Reagent.-Van Slyke and Hawkins tungstic acid. (Twenty-five ml. of 2/3 N sulfuric acid and 25 ml. of 10-percent sodium tungstate are combined and diluted to 225 ml. with water.) This reagent is satisfactory for 1 week. Turbidity due to precipitation of tungstic acid does not interfere with preparation of the filtrate.
Procedure.-To 1 volume of blood or plasma in a flask are added9 volumes
325
TABLE 118.-NORMAL VALUES USED INTHIS STUDY
of the tungstic acid reagent, the mixture is allowed to stand for 10minutes and is then filtered.
TRICHLORACETIC ACID FILTRATES
Reagents.-Trichloracetic acid, 10-percent solution,15-percent solution, and 20-percent solution. (Prepared by titration.)
Procedure.-Prepare filtrates (as required by the analysis to be performed)
326
Determination of Blood and Plasma Volume
MODIFICATION OF GREGERSENMETHOD
Blood and plasma volume was determined in this study by modification of the method developed by Gregersen1 2 primarily for use of the Armed Forces. The dye T-1824 was used and the basic principles of the method were followed.
The Gregersen method, in brief, consists in injecting a known quantity of dye into the antecubital vein, waiting about twenty minutes for the dye to be distributed through the circulating blood, and taking three or four samples of blood at 20-minute intervals. The plasma is separated and its concentration of dye is measured and plotted against time. The curve so obtained is extrapolated back to zero time to correct for dye lost during the mixing period. This value at zero time gives the theoretical concentration of dye that would have occurred in the plasma if uniform mixing had been effected at the instant of injection and none of the dye had been excreted. The total blood volume is calculated from the plasma volume (measured by the dye) and the hematocrit value.
Experience with the method revealed two serious objections, one practical and one technical. The practical objection was that the method was too time-consuming for use with battle casualties before operation; therefore, a more rapid procedure was sought. This will be discussed later. The technical flaw in the procedure was that the difference in turbidity between the blank, dye-free plasma and the dye-containing samples yielded spectrophotometric readings which had to be resolved as amount of dye plus or minus turbidity. Plotted points using such readings rarely indicated excretion of dye as an exponential function, and very often, when considerable variations in turbidity existed, would lead to gross errors of reading at zero time. Corresponding errors resulted in the calculation of the blood volume.
The cause of this turbidity, which varies during the course of a determination, has not been ascertained. The plasma, however, does not clear upon centrifugation. The following observations made the application of a turbidity-correction
1GREGERSEN, M. I.; GIBSON, J. G., and STEAD,E. A.: Plasma volume determination with dyes: errors in colorimetry; use of the blue dye T-1824. Am. J. Physiol. 113: 54-55, Sept. 1, 1935.
2GREGERSEN, M. I.: A practical method for the determination of blood volume with the dye T-1824; survey of the present basis of the dye-method and its clinical applications. J. Lab. & Clin. Med. 29:1266-1286, December 1944.
327
factor reasonable: (1) The reading of turbidity at 620 mµ was almost the same as at 680 mµ, while (2) the dye reading at 680 mµ was ¼ the reading at 620 millimicrons.
If the dyed plasma, therefore, is less turbid than the blank, dye-free plasma, the difference in readings of the dyed plasma at 620 mµ and 680 mµ expressed as OD (optical density), multiplied by4/3, would give the corrected value for the dye only.
Example:
OD at 620 mµ . . . 0.309
OD at 680 mµ . . . 0.055
OD corrected (0.309 - 0.055) x 4/3 = 0.340
If the dyed plasma is more turbid than the dye-free plasma, which it is if the reading of optical density at 680 is more than ¼ the reading at 620, a similar correction is made.
Example A:
OD at 620 mµ . . . 0.300
OD at 680 mµ . . . 0.091
OD corrected (0.300 - 0.091) x 4/3 = 0.279
Example B:
OD at 620 mµ = 0.409
OD at 680 mµ = 0.188
OD corrected (0.409 - 0.188) x 4/3 = 0.295
When the dyed plasma and the blank plasma are of the same order of turbidity, no correction factor is necessary.
The application of the correction factor for turbidity materially improved the character of the blood-volume curves, and indicated that the excretion of the dye approximated an exponential function.
Practically, the use of four points to determine blood volume is too time-consuming to be used in battle casualties before operation. Therefore, a more rapid method was sought, and the accuracy of a blood volume determination based on only one blood sample was studied.
Since the excretion of the dye followed an exponential curve, and the log of the concentration of the dye plotted against time formed a straight line, it remained only to determine the constancy of the slope of the disappearance curve, and to ascertain 1 point on the line, at a specified time, to calculate the optical density (OD) at zero time. This was done in 68 cases in which blood volumes had been determined by using 3-point, 4-point, and 5-pointcurves to establish the optical density at zero time.
First it was necessary to consider the factor of albuminuria. Because the dye T-1824 is thought to be bound to the plasma albumin, a variability of slope
328
according to the presence or absence of albuminuria was expected. Such a relationship was demonstrated by grouping the dye disappearance-rate slopes in 67 cases according to the amount of albumin in urine specimens obtained in these cases at about the time the blood volume was determined. The disappearance of dye from plasma was expressed by the slope factor OD 0 minutes/OD 60 minutes.
If the slope factor is divided into 1,000 and multiplied by 100, it gives the percentage of dye remaining in the plasma 1 hour after injection; subtraction of the result yields the percentage of dye lost in 1 hour. The average percentage of dye lost in 1 hour in the urines of patients with no urinary suppression and with albuminuria (Group V), as compared with the average loss in 1 hour in the other four groups combined, would indicate that the dye, bound to albumin, is lost through the urine in this manner (Table 119).
TABLE 119.-COMPARISON OF ALBUMIN LOSS IN URINE WITH PLASMA DYE LOSS-AVERAGE OF 67 CASES
329
When the cases in Groups I through IV were combined and averaged, a weighted slope of 1.112 was obtained, corresponding to a 10-percent loss of dye per hour, or a change per minute of 0.00187 or .1112/60. It was possible, then, to calculate the OD at zero time, when the OD at a specific time was known, by multiplying by 0.00187 the interval (in minutes) between injecting the dye and taking the sample, and adding 1 to this figure. The OD at zero minutes was obtained by multiplying this value by the observed OD corrected for turbidity.
Example:
OD 30 minutes (corrected): 0.317
1. 30 x 0.00187 = 0.0561
2. 1 + 0.056 = 1.056
3. 0.317 x 1.056 = 0.335 (OD zero time)
To test the validity of this procedure, the first point of each of the 68 multiple-point blood volume tests was taken and the blood volume was calculated from it and compared with the blood volume obtained by determining the disappearance curve from multiple points. The results are indicated in Table 120.
TABLE 120.- RELATION OF CALCULATION OF SINGLE-POINT TO MULTIPLE-POINT METHOD-68 CASES
According to these data, in 69 percent of the 68 cases the calculation of blood volumes was higher by the single-point method, in 31 percent it was lower, and was within 100 ml. in 56 percent. In 90 percent of all cases it was within 300 ml. of the calculation obtained by the multiple-point method. In this series the value determined by the one-point method was clinically unsatisfactory in one case (960 ml. too high). The second point in this case
330
yielded a value 330 ml. too high. This series demonstrated that the blood volume determined by the one-point test compares favorably with that obtained by the multiple-point test.
PROCEDURE FOR DETERMINATIONOF BLOOD AND PLASMA VOLUME
Reagents
1. T-1824 solution, 1 mg. per milliliter. (The contents of ten 5-ml. ampules of 0.5-percent T-1824 are removed and made up to a250-ml. solution, using sterile technique.)
2. Standard copper sulfate solutions (specific gravity series for determination of hematocrit value).
3. Sodium chloride, 0.9-percent solution.
Procedure
A sterile 10-ml. syringe is filled with exactly 10 ml. of T-1824 and placed where it will be readily available. About twenty milliliters of blood are drawn from the antecubital vein with a sterile syringe, leaving the needle in the vein. Exactly 5 ml. of blood are measured into a specially oxalated bottle for determination of the hematocrit value, and the remaining blood is transferred to a lithium oxalate bottle. This is the blank tube. The syringe containing the dye is carefully attached to the needle remaining in the vein, and all the dye is injected. (Any indication of pain by the patient during the injection of the dye should be regarded as evidence that some dye is passing outside the vein, thus invalidating the analysis.)The exact time of injection is noted. After an interval of from 20 to 40 minutes, 15 ml. of blood are drawn from the antecubital vein of the opposite arm and placed into a lithium oxalate bottle. This is the dye-containing tube. Again the exact time the blood is drawn is noted.
The hematocrit value is determined from the 5-ml. sample (the blank blood), using the copper sulfate method of Phillips et al.3All the samples are centrifuged and the supernatant plasma is separated. The two tubes of blank plasma are pooled, at least 5.5 ml. are placed in a 19- by 150-mm. Coleman cuvette, and the same quantity of the dye-containing plasma is placed in a similar cuvette. (In the event that the amount of plasma is inadequate, dilutions
3PHILLIPS, R. A.; VAN SLYKE, D. D.; DOLE, V.P.; EMERSON, K., JR.; HAMILTON, P. B., and ARCHIBALD, R. M.: Copper sulfate method for measuring specific gravities of whole blood and plasma. BUMED News Letter, U.S. Navy, June 25, 1943, p. 1-16.
331
are made with 0.9-percent saline solution, treating both tubes in the same manner.)
The blank tube is set to read at 100-percent transmission at 620 mµ in the spectrophotometer and the optical density of the plasma in the dye tube is noted. This procedure is repeated at 680 millimicrons. Exactly 1 ml. of T-1824 solution is diluted to 500 ml. with water, placed in a matched cuvette, and, blanking out with distilled water, the optical density at 620 mµ is determined.
Calculation
1. From the readings at 620 mµ and 680 mµ the corrected optical density (OD) is calculated as discussed previously.
2. The optical density is calculated at zero minutes, using the factor for the number of minutes after injection as previously discussed.
3. Plasma volume:
ODo = corrected optical density at zero minutes for dyed plasma.
ODdye = optical density of (1:500) dilution of dye that was injected for test.
Plasma volume = ODdye/ODo x 500 x 10.
(The figure of 500 represents the dilution factor of the dye as read in the instrument, and the figure 10 is the number of milliliters injected.)
4. Blood volume:
100 minus the hematocrit value = percentage of plasma(% Pl)
Blood volume = Plasma volume/% Pl x 100
Summary
1. The technique for determining the circulating blood volume by means of the dye T-1824 and a spectrophotometer is described.
2. The correction for variable turbidity of samples is described.
3. The disappearance of the dye in battle casualties was 10 percent of the injected substance at the end of 1 hour.
4. Albuminuria increased the disappearance rate.
5. The feasibility of blood volume determinations based on only one dye-containing sample is demonstrated.
332
Blood Chemistry
NONPROTEIN NITROGEN PRODUCTS
Nonprotein Nitrogen in Plasma-Modified from Koch and McMeekin4
Reagents
1. Sulfuric acid, 50-percent aqueous solution by volume.
2. Potassium persulfate, saturated solution. (Seven Gm.in 100 ml. of water.)
3. Potassium mercuric iodide for Nessler`s solution: (a)Using a 1-liter Erlenmeyer flask, 22.5 Gm. of iodine are dissolved in 20ml. of water containing 30 Gm. of potassium iodide. (b) After the solution is complete, 30 Gm. (about 2.5 ml.) of mercury are added and the mixture is shaken vigorously in order to break the mercury into globules, cooling it from time to time by immersing the flask in cold water. The shaking is continued until the supernatant fluid has lost all color due to iodine.(c) The supernatant is decanted from the excess mercury and tested for free iodine by adding a drop or two of the solution to 1 ml. of a 1-percent starch solution. If the result of the starch test for iodine is negative, a few drops of an iodine solution of the same concentration as described in (a) are added until a faint excess of iodine can be detected by the starch test. (d) The double iodide solution is diluted to 200 ml. with distilled water and mixed thoroughly.
4. Nessler`s reagent. (By titration a 10-percent sodium hydroxide solution is accurately prepared from a saturated solution of sodium hydroxide that has been allowed to stand until all carbonates have settled. To 975 ml. of this solution is added the entire solution (200ml.) of potassium mercuric iodide prepared as described, after which it is mixed thoroughly and allowed to settle.)
5. Ammonium sulfate standard solution. (Prepared by dissolving4.716 Gm. of pure, dry ammonium sulfate in 0.2 N sulfuric acid and making up to a volume of 1,000 ml. with the 0.2 N sulfuric acid (1 ml. = 1 mg. of nitrogen).)
6. Dilute nitrogen standard solution. (Five ml. of stock standard solution is diluted to 100 ml. with 0.2 N sulfuric acid (3 ml.= 0.15 mg. nitrogen).)
Procedure
To 2.5 ml. of protein-free tungstic acid plasma filtrate in an ignition tube graduated at 35 ml. is added 1 ml. of 50-percent sulfuric acid solution, together with a glass bead to prevent bumping, and it is boiled vigorously until it becomes brown and dense white fumes appear. A funnel is then placed in the tube and the solution is digested for about one minute, when the flame and funnel are removed, 5 drops of potassium persulfate are added, and the mix-
4In HAWK, P. B., and BERGEIM, O. Practical Physiological Chemistry. 10th ed. Philadelphia, Blakiston, 1931, p. 415.
333
ture is boiled gently for several minutes. If a brown color persists, another 5 drops of potassium persulfate are added and the mixture is again boiled gently. (A greenish-yellow color at this point indicates an excess of tungstic acid. This color will clear up after the addition of the Nessler`s reagent.) It is cooled, diluted to the 35-ml. mark with water, and mixed by inversion.
Into an identical ignition tube are placed 3 ml. of working standard and 1 ml. of 50-percent sulfuric acid solution; this is made up to the 35-ml. mark with water and mixed by inversion. Into a third ignition tube is placed 1 ml. of the sulfuric acid solution, water is added to the 35-ml.mark, and it is mixed by inversion. This is the blank. Next, 3.5 ml. each of the sample, the standard, and the blank are transferred to a small cuvette(12 by 75 mm.), 1.5 ml. of Nessler`s reagent is added, the contents are mixed by inversion, and read in the Coleman Junior Spectrophotometer at 440 mµ on the optical density scale, blanking out with the blank solution.
If the nonprotein nitrogen value is high, 2 ml. of the solution and 1.5 ml. of the blank are nesslerized. In this case the final value is multiplied by seven-fourths. Other appropriate dilutions that bring the color intensity into the standard range can be used.
Calculation
The working nitrogen standard is equivalent to 60 mg. of nitrogen per100 ml. of plasma. (Rs = OD of the standard.
Ru = OD of the sample.)
60/Rs = x/Ru
60 x RU/Rs = mg./100 ml. nitrogen in plasma sample.
Comment
The method as modified has the following advantages: (1) Nessler`s solution is used sparingly; less than 10 percent of the quantity used in the standard procedure is necessary. (2) The procedure is expedited by the digestion of half the quantity of filtrate ordinarily used. (3) An objective reading of the nesslerized solutions increases the accuracy of reading the yellow color. (4) In the event the nonprotein nitrogen level is extremely high, a further dilution of the initial digestion can be made, rather than repeating the entire analysis. (5) The use of saturated potassium persulfate in the oxidation provides a substance which is nitrogen-free, stable, and unlike superoxol, is non-injurious.
334
Creatinine in Plasma-Modified from Folinand Wu5
Reagent.-Alkaline picrate solution. (Five volumes of saturated picric acid are mixed with 1 volume of 10-percent sodium hydroxide solution. This is freshly prepared before each series of analyses.) A reference curve is prepared from standard creatinine solutions read on the spectrophotometer at 500 mµ after following the conditions of the test.
Procedure.-Five ml. of tungstic acid plasma filtrate are placed in one cuvette, and 5 ml. of water in another. To each of the samples and the water blank are added 2.5 ml. of alkaline picrate solution and they are allowed to stand for 10 minutes. The blank is set at 100-percent transmission and the percentage transmission of each sample is read at 500 millimicrons.
Calculation.-Reference of the observed percentage transmission to the standard curve gives the milligrams of creatinine per 100 ml. of plasma. If very high creatinine values are anticipated, appropriate dilutions of the tungstic acid filtrate are made with water before addition of the alkaline picrate.
Uric Acid in Plasma-Modified from Folin6
Reagents
1. Standard solution of uric acid. (Exactly 1 Gm. of uric acid is transferred to a 1-liter volumetric flask. To 0.5 Gm. of lithium carbonate in a beaker, 150 ml. of water are added and this solution is heated to 60° C. until all the carbonate has dissolved. All of the hot carbonate solution is then added to the uric acid in the volumetric flask. As soon as a clear solution is obtained, it is cooled, diluted to about five hundred ml. with water, and 25 ml. of formaldehyde are added. This is well mixed and 3 ml. of glacial acetic acid are added. The mixture is shaken to remove most of the carbon dioxide, diluted to 1 liter, mixed, and stored in brown bottles.)
2. Working standard. (Immediately before each series of analyses, 0.4 ml. of the standard solution is diluted to 100 ml. with water.)
3. Five-percent sodium cyanide solution.
4. Uric acid reagent. (To 100 Gm. of sodium tungstate(molybdate-free) in a 500-ml. Florence flask is added dilute phosphoric acid, made by dissolving 33 ml. of 85-percent phosphoric acid in 150 ml. of water, and the solution is mixed. Several glass beads are added to the flask and the mixture is boiled gently for 1 hour, using a funnel containing a flask of cold water as a condenser. It is decolorized with a little bromine water, the excess bromine is boiled off, and the mixture is cooled and diluted to a volume of 500 ml.)
5In HAWK, P. B., and BERGEIM, O. Practical Physiological Chemistry. 10th ed. Philadelphia, Blakiston, 1931, p. 421-423.
6In SIMMONS, J. S., and GENTZKOW, C. J. Laboratory Methods ofthe United States Army. Philadelphia, Lea & Febiger, 1944, p. 207.
335
Procedure
To 1 ml. of tungstic acid filtrate in a cuvette are added 3 ml. of water. Into another cuvette is pipeted 1 ml. of dilute standard, and 3 ml. of water are added. This is the standard solution corresponding to 4 mg. of uric acid per 100 ml. of plasma. Four ml. of water in a third cuvette constitutes the blank tube. To each of the samples, the uric acid standard, and the blank tube, 4 ml. of sodium cyanide are added, using an automatic pipet, and the solutions are mixed, after which 2 ml. or uric acid reagent are added to each tube, and the solutions are again mixed and are allowed to stand for 30 minutes. The blank is set at 100-percent transmission on the spectrophotometer and the optical density of the standard and each of the samples at 650 mµ is noted.
Calculation
The calculation of milligrams per 100 milliliters of plasma is obtained by setting up a proportion comparing the optical density of the standard of known strength with the observed reading of the sample.
Example:
OD of sample . . . 0.150
OD of standard . . . 0.200
Standard = 4 mg./100 ml.
Sample (calculated) = 3 mg. of uric acid per 100 ml. of plasma.
Comment
The advantages of the method as modified are that it (1) yields a non-clouding color development when sodium cyanide and phosphotungstic acid are used,(2) avoids the danger of color development varying with the temperature by the preparation of standard and blank at the same time and by reading the color on the optical density scale of the spectrophotometer, and (3)insures against decomposition of the working standard by preparation of a fresh standard before each series of analyses.
Urea Nitrogen in Plasma-Modified from Karr 7
Reagents
1. Urease solution. (A mixture of 0.3 Gm. of double-strength urease in 2.5 ml. of water and 7.5 ml. of glycerin is centrifuged and decanted. The supernatant solution is the urease extract and lasts for at least 3months.)
7In HAWK, P. B., and BERGEIM, O. Practical Physiological Chemistry. 10th ed. Philadelphia, Blakiston, 1931, p. 418.
336
2. Acetate buffer solution. (To 15 Gm. of sodium acetate dissolved in 50 ml. of water is added 1 ml. of glacial acetic acid, and the mixture is diluted to 100 ml. with water.)
3. Dilute standard nitrogen solution. (Same as for nonprotein nitrogen.)
4. Potassium mercuric iodide. (Same as for nonprotein nitrogen.)
5. Urea Nessler`s reagent. (Thirty ml. of potassium mercuriciodide are mixed with 30 ml. of water and 140 ml. of 5-percent sodium hydroxide solution are added.)
6. 2/3 N sulfuric acid.
7. Sodium tungstate, 10-percent solution.
Procedure
To 1 ml. of plasma in a tube are added 6.7 ml. of water, 2 drops of urease solution, and 4 drops of acetate buffer, and the tube is incubated at 40° to 50° C. for 15 minutes. One ml. each of the sulfuric acid and the sodium tungstate solution are added, the solution is mixed, allowed to stand for several minutes, and filtered. Into another tube are placed 2 ml. of filtrate and 7 ml. of water. Into a tube graduated at 22.5 ml. are placed 1.5 ml. of the working nitrogen standard, the solution is diluted to the mark, mixed, and 9 ml. of this dilute standard is placed in a tube. To each of the samples and the dilute standard solution is added 1 ml. of urea Nessler`s reagent, they are mixed and read in the colorimeter.
Calculation
The unknown is set at 15 mm. and the reading of the standard will be the milligrams of urea nitrogen per 100 ml. of plasma. In the event thata high urea nitrogen is expected, aliquots of the 2-ml. sample of filtrate are taken and the contents of the tube made up to 9 ml. with water. The observed level is then multiplied by the proper factor.
Example: 0.5 ml. taken instead of 2.0 ml.; multiply answer by 4 for mg. of urea nitrogen per 100 ml. of plasma.
A urease blank should be determined about every 3 days. The urease blank usually averaged between 2 and 3 mg. expressed as urea nitrogen per 100ml. of plasma and was subtracted from the observed values.
Comment
The method as modified has the following advantages: (1) It yields anon turbid, stable solution upon direct nesslerization; (2) the reagents are stable at room temperature and are used sparingly, and (3) if the urea nitrogen level
337
is extremely high, a further dilution of the initial filtrate of the incubation mixture can be made, rather than repeating the entire analysis.
ACID-BASE ANALYSES
Blood pH (from Hawkins, Hastings, and Sendroy8)
Preparation of the bicolor standards was taken from Peters and Van Slyke`s Quantitative Clinical Chemistry (cited below) p. 797, Table 65.The preparation of the reagents (p. 796) and Hawkins` modification (p.801) for using a sample of whole blood were also followed.
Procedure
The phenol red tube and the saline tube are prepared immediately before the analysis, using tubes similar to those for the preparation of standards.(Phenol red tube: After placing 5 ml. of freshly adjusted saline solution (which contains 11 ml. of 0.0075-percent phenol red solution per 100 ml.) in a tube, about one-quarter inch of liquid petrolatum is stratified above this solution. Saline tube: Five ml. of freshly prepared saline are put into a similar tube.)
Drawing blood samples: A glass bead is placed in the barrel of a 2-ml. syringe with needle attached, about 0.5 ml. of sterile liquid petrolatum and a small drop of saturated potassium oxalate are added, and the plunger is inserted in the syringe. The syringe is inverted so that the needle is pointing upward, the droplet of potassium oxalate is allowed to fall to the bottom of the solution, and all the air and excess petrolatum are slowly expressed until the movement of the plunger is arrested by the glass bead. The excess petrolatum is wiped off the needle, a blood sample of about 1.5 to 2 milliliters is taken, and the syringe is inverted several times to insure mixing with the oxalate. After waiting a moment for the petrolatum to stratify to the top of the syringe, the needle is placed under the petrolatum layer of the phenol red tube and exactly 0.5 ml. of blood is expressed into the tube. In a similar manner 0.5 ml. of blood is placed in the saline tube. The petrolatum is siphoned off from the phenol red tube, which is then sealed with ¼ inch of paraffin, and the contents of both tubes are mixed by inversion and centrifuged.
8In PETERS, J. P., and VAN SLYKE, D. D. Quantitative Clinical Chemistry. vol. II: Methods. Baltimore, Williams & Wilkins,1932, p. 796-801.
338
Color comparison is made by arrangement of the tubes in the comparator as illustrated in Fig. 87 of Peters and Van Slyke`s Quantitative Clinical Chemistry. Readings are made between 18° and 20° C., noting the temperature in the saline tube.
Correction of Observed pH to pH at 38° C.
Since the standards were prepared to read pH at 38° C., it is necessary only to subtract the observed temperature from 38° C., multiply this difference by 0.005 and subtract this product from the observed pH to obtain blood pH at 38° Centigrade.
Example:
1. Observed pH 7.48 at 20° C.
2. 38 - 20 = 18
3. 18 x 0.005 = 0.09
4. 7.48 - 0.09 = pH 7.39 at 38° C.
Normal controls are run with each series of analyses.
Serum Sodium-Modified from Weinbach`s Modification of Butler and Tuthill`s Method 9
Reagents
1. Trichloracetic acid, 20-percent solution.
2. Sodium reagent (uranyl zinc acetate). ((a) Uranium acetate, 38.5 Gm., and glacial acetic acid, 14 ml., are dissolved in 150ml. of distilled water with the aid of heat. (b) Zinc oxide, 37.5 Gm., and glacial acetic acid, 63 ml., are dissolved in 150 ml. of distilled water with the aid of heat. (c) The two solutions are combined, mixed, cooled, and made up to 500 ml. with distilled water. (d) This solution is transferred to a reagent bottle, about 0.5 Gm. of the salt sodium uranyl zinc acetate is introduced, and this mixture is shaken to effect saturation with the sodium uranyl zinc acetate.)
3. Standard sodium solution, 330 mg. of sodium per 100milliliters. (Sodium chloride, 0.840 Gm., is diluted to 100 ml. with water and stored in a paraffin-lined bottle.)
4. 95-percent ethyl alcohol.
5. Acetone wash. (Sodium uranyl zinc acetate, 0.5 Gm., is introduced into a bottle containing about one liter of acetone, the bottle is well shaken and allowed to stand at least overnight before using.)
6. A 0.0348 N solution of sodium hydroxide.
9In HAWK, P. B., and BERGEIM, O. Practical Physiological Chemistry. 11th ed. Philadelphia, Blakiston, 1937, p. 472-473.
339
7. Sodium uranyl zinc acetate. (One ml. of a 5-percent solution of sodium chloride is added to 15 ml. of the sodium reagent in a 50-ml. Erlenmeyer flask, and 1 ml. of 95-percent ethyl alcohol is added at 5-minute intervals until 5 ml. have been added. The mixture is filtered, using suction, and the precipitate of sodium uranyl zinc acetate is washed three times with alcohol and three times with ether, sucking dry after each washing.)
Preparation of Glassware.-Two clean graduated centrifuge tubes for each determination and two for the standard are prepared by rinsing them four times with distilled water and drying in an oven.
Procedure
One volume of serum, 3 volumes of water, and 1 volume of 20-percenttrichloracetic acid are mixed in a tube by inversion, and the process is repeated, using 1 volume of the standard sodium solution instead of serum. Into each of two of the specially prepared centrifuge tubes are placed 0.5 ml. of the serum filtrate, and into each of the two other specially prepared centrifuge tubes 0.5 ml. of the dilute standard. Five ml. of filtered sodium reagent are then added to each tube, followed by 0.3 ml. of 95-percent ethyl alcohol at 5-minute intervals until 2.1 ml. have been added to each, when the supernatant fluid is centrifuged and decanted, allowing the tubes to drain and taking care not to dislodge the residue. Five ml. of filtered acetone wash are blown into the residue, the tubes are centrifuged, and the supernatant is decanted and drained. This process is repeated two more times, making three washings in all. Using 25 ml. of distilled water, the residue is dissolved and transferred quantitatively to a 125-ml. Erlenmeyer flask and titrated with 0.0348 N sodium hydroxide using phenolphthaleinas the indicator.
Calculation
1 ml. of 0.0348 N sodium hydroxide = 100 mg. of sodium per 100 ml. of serum.
Example:
|
Titration of Sample I |
Sample II |
Average | |
|
Serum |
3.43 |
3.45 |
3.44 or 344 mg./100 ml. |
|
Standard |
3.38 |
3.36 |
3.37 or 337 mg./100 ml. |
Actual strength of standard: 330 mg./100 ml.
Determined strength of standard: 337 mg./100 ml.
Difference (blank): 7 mg./100 ml.
Therefore, 344 - 7 = 337 mg. of sodium per 100 ml. of serum.
Mg./100 ml. sodium x 10/23 = milliequivalents of sodium.
340
Comment
The modified method used was further modified (1) by changing the strength of the sodium hydroxide used, thus simplifying the calculation, (2) byusing a standard of known sodium concentration to ascertain the reagent blank, and (3) by an additional acetone washing.
Serum Potassium (Kramer and Tisdall10)
The standard procedure was followed, with duplicate analyses of each sample and potassium standards for every analysis.
Serum Calcium (Clark-Collip Modification of Kramer and Tisdall Method11)
The standard procedure was followed.
Magnesium in Plasma-Modified from Herschfelder and Serles12
Reagents
1. Titan yellow, 0.05-percent solution. (This keeps for about two weeks.)
2. Sodium hydroxide, 10-percent solution.
3. Trichloracetic acid, 10-percent solution.
4. Stock magnesium standard solution. (One Gm. of magnesium sulfate heptahydrate is dissolved with a little water and then made up to a 100-ml. solution.)
5. Working magnesium standard solution. (1.45 ml. of stock standard diluted to 100 ml. with water. (7 milliliters = 0.1 mg. magnesium.)A standard reference curve is prepared, using this solution according to conditions of the test. The color is read at 535 mµ in the spectrophotometer.)
Procedure
To 2 ml. of plasma are added 4 ml. of water and 4 ml. of 10-percenttrichloracetic acid. The solution is mixed, allowed to stand for several minutes,
10In TODD, J. C., and SANFORD, A. H. Clinical Diagnosis by Laboratory Methods. 10th ed. Philadelphia, W. B. Saunders, 1943, p. 420-421.
11In HAWK, P. B., and BERGEIM, O. Practical Physiological Chemistry.10th ed. Philadelphia, Blakiston,
1931, p. 460-461.
12HERSCHFELDER, A. D., and SERLES, E. R.: A simple adaptation of Kolthoff`s colorimetric method for the determination of magnesium in biological fluids. J. Biol. Chem. 104: 635, March 1934.
341
centrifuged, and filtered. To 5 ml. of plasma filtrate in a cuvette,1.6 ml. of water is added, and 7 ml. of water in another cuvette serves as the blank. One ml. of titan yellow is then added to each of the samples and to the blank. Two ml. of the sodium hydroxide solution are added to the blank tube, the contents are mixed, and the tube is set to read at 100-percent transmission on the spectrophotometer at 535 millimicrons. Similarly, 2.4 ml. of the sodium hydroxide solution are added to each of the samples, and the solution is mixed and read immediately on the spectrophotometer at 535 millimicrons.
Calculation
Milligrams of magnesium per 100 ml. of plasma are determined by reference of the observed percentage transmission to the standard curve.
Comment
This method is a simple, rapid procedure. Recoveries of added magnesium and comparisons of normal range of plasma magnesium with that of other methods (1.5-2.0 mg. per 100 ml.) indicate its accuracy.
Phosphorus in Plasma-Modified from Bodansky13
The method was modified by making up the standard in trichloracetic acid. This permitted of more exact color comparison and eliminated theneed for the two molybdate solutions which the original method demands.
Carbon-Dioxide Combining Power of Plasma
(Van Slyke and Cullen14)
Chlorides in Plasma (Schales and Schales15)
Plasma chlorides were determined by the method of Schales and Schales.
13In TODD, J. C., and SANFORD, A. H. Clinical Diagnosis by Laboratory Methods. 10th ed. Philadelphia, W. B. Saunders, 1943, p. 404-411.
14The procedure was followed as described in Methods for Laboratory Technicians, War Department Technical Manual 8-227, October 1946, p. 123-129.
15In SIMMONS, J. S., and GENTZKOW, C. J. Laboratory Methods of the United States Army. Philadelphia, Lea & Febiger, 1944, p. 209.
342
Lactic Acid in Plasma-Modified from Mendeland Goldschieder16
Reagents
1. Metaphosphoric acid, 5-percent solution, prepared daily.
2. Copper sulfate, 15 percent by weight of pentahydrate.
3. Blank-free concentrated sulfuric acid. (The quality of the sulfuric acid should be such that no yellow color develops on the addition of 0.1 ml. of 0.125-percent veratrole to 3 ml. of acid. A good reagent grade of sulfuric acid is satisfactory.)
4. Lactic acid, 100 mg. per 100 ml., prepared from lithium lactate.
5. Sodium fluoride, 0.1-percent solution.
6. Veratrole, 0.125 percent in absolute alcohol.
Procedure
To 1 ml. of plasma separated from freshly drawn blood are added 5 ml. of water, 1 ml. of sodium fluoride, and 1 ml. of metaphosphoric acid. The whole is shaken vigorously, allowed to stand for several minutes, and filtered. To 4 ml. of the protein-free filtrate in a centrifuge tube are added 1ml. of copper sulfate solution and 1 Gm. of calcium hydroxide, the mixture is allowed to stand about 30 minutes, shaking several times, and is then centrifuged. The pellicle of copper hydroxide is broken with a glass rod and the supernatant is decanted into another tube and centrifuged again, resulting in a clear, sugar-free filtrate. The standard lactic acid solution is diluted 1:10, corresponding to 100 mg. of lactic acid per 100 ml. of plasma, according to the conditions of the test. Weaker dilutions corresponding to 75, 50, 25, and 12.5 mg. of lactic acid per 100 ml. of plasma are also prepared.
To 0.5 ml. of the clear sugar-free filtrate (obtained by centrifugation only), to 0.5 ml. of each standard, and to 0.5 ml. of water in a carefully cleaned test tube, 3 ml. of concentrated sulfuric acid are slowly added while the tubes are cooled in cold water. The tubes are then placed in a boiling water bath for exactly 4 minutes, removed and immersed in cold water for 5 minutes. To each tube 0.1 ml. of the veratrole solution is added, and the solution is mixed and allowed to stand for 20 minutes, after which it is decanted into small cuvettes (12 by 75 mm.) and read in the spectrophotometer at 545 mµ, blanking out with the water reagent blank and reading the optical density scale.
16In PETERS, J. P., and VAN SLYKE, D. D. Quantitative Clinical Chemistry. vol. II: Methods. Baltimore, Williams & Wilkins,1932, p. 618-620.
343
Note: In the process of color development, a brown color may form in addition to the pink of the test color. This is due to unclean glassware and contaminated filtrate. In these instances the analysis is repeated.
Calculation
A proportion is set up comparing the reading of the sample with that of the nearest standard.
Comment
The test was set up on the spectrophotometer, and readings were made on the optical density scale, using a series of standards with each run, since color development is not reproducible from day to day as required for using a permanent chart. The color development does not satisfactorily follow Beer`s law, and the optical density reading of the closest standard was used in calculating the value of the sample.
The use of 1 ml. of sodium fluoride in the dilution of the plasma permits preservation of the lactic acid level until a series of samples has accumulated.
GLUCOSE IN PLASMA
The standard procedure of Folin and Wu17 was followed for the determination of glucose in plasma.
SULFONAMIDES IN WHOLEBLOOD
The method of Bratton and Marshall18 was followed.
DETERMINATION OF METHEMOGLOBIN
The method of Paul and Kemp19 was followed.
17In SIMMONS, J. S., and GENTZKOW, C. J. Laboratory Methods of the United States Army. Philadelphia, Lea & Febiger, 1944,p. 207-208.
18In SIMMONS, J. S., and GENTZKOW, C. J. Laboratory Methods of the United States Army. Philadelphia, Lea & Febiger, 1944, p. 219-220.
19PAUL, W. D., and KEMP, C. R.: Methemoglobin; a normal constituent of blood. Proc. Soc. Exp. Biol. & Med. 56: 55-56, 1944.
344
PLASMA BILIRUBIN (VANDEN BERGH)
The method of Evelyn and Malloy20 was followed.
HEMOGLOBIN, HEMATOCRIT, ANDPLASMA PROTEIN
The method of Phillips et al.21 for the calculation of hemoglobin, hematocrit value, and plasma proteins by means of copper sulfate was followed with the exception that, since a chemical balance was available, all the solutions were checked and standardized so that they were correct to within ±2 units in the fourth decimal place, using a 25-ml. pyknometer and water at the same temperature as the standard solution. Each bottle was prepared in 1-liter quantity and replacements were made from this stock. Bottles were prepared for each unit difference in the third decimal place.
PLASMA HEMOGLOBINDETERMINATION
Plasma Hemoglobin-Modified from Bing andBaker22
Reagents
1. Benzidine reagent. (Five Gm. of a good quality of benzidine are dissolved in 50 milliliters of glacial acetic acid, warming gently to effect solution. The mixture is cooled, diluted to 250 ml. with distilled water, about 2 Gm. of decolorizing charcoal are added, and the solution is thoroughly mixed, allowed to stand for approximately 10 minutes, and filtered into a brown bottle.)
2. Hydrogen peroxide, 3-percent solution.
3. Hemoglobin standard solution. (A 20-mg. per 100 ml. solution of hemoglobin is prepared in 1-percent boric acid by diluting blood of known hemoglobin content.)
4. Acetic acid, 20-percent solution.
Procedure
To 0.2 ml. of each sample and of the standard in separate tubes are added
20In SIMMONS, J. S., and GENTZKOW, C. J. Laboratory Methods of the United States Army. Philadelphia, Lea & Febiger, 1944,p. 214-215.
21PHILLIPS, R. A.; VAN SLYKE, D. D.; DOLE, V. P.; EMERSON, K.,JR.; HAMILTON, P. B., and ARCHIBALD, R. M.: Copper sulfate method for measuring specific gravities of whole blood and plasma. BUMED News Letter, U.S. Navy, June 25, 1943, p. 1-16.
22BING, F. C., and BAKER, R. W.: The determination of hemoglobinin minute amounts of blood by Wu`s method. J. Biol. Chem. 92: 589-600,August 1931.
345
2 ml. of the benzidine reagent, and each is thoroughly mixed. One ml. of the 3-percent hydrogen peroxide is then added to each tube and they are allowed to stand for 30 minutes, at the end of which time the mixtures are diluted with 6.8 ml. of the acetic acid and allowed to stand until all the tubes have developed the red color (about 30 minutes), when they are compared in the colorimeter.
Calculation
The sample is set on 20 millimeters. The reading of the standard equals milligrams of benzidine-reacting substance per 100 ml. of plasma. As has been explained in Chapter VIII of the text, this entire benzidine-reacting substance was termed "plasma hemoglobin" because a means forits further breakdown was not available to us.
Liver Function Test
Bromsulfalein Test-Modified from Rosenthal23
Reagents
Bromsulfalein, 5-percent solution, in sterilized, sealed ampules.
Sodium hydroxide, 10-percent solution.
3. Sodium chloride, 0.9-percent solution.
Procedure
The patient`s weight is recorded in kilograms and the amount of dye to be injected is calculated on the basis of 5 mg. per Kg. of body weight. A simple procedure is to divide the body weight in kilograms by 10 to yield the exact amount in milliliters of bromsulfalein to be used for injection. The required amount of dye is drawn into a 10-ml. syringe and slowly injected into a vein in the patient`s arm, the exact time of injection being recorded. Forty-five minutes after injection, a sample of blood from the opposite arm is collected in the standard lithium oxalate bottle, the blood specimen is centrifuged, and the plasma is collected.
23In TODD, J. C., and SANFORD, A. H. Clinical Diagnosis by Laboratory Methods. 10th ed. Philadelphia, W. B. Saunders,1943, p. 428-429.
346
To 1 ml. of plasma placed in a cuvette 5 ml. of a 0.9-percent solution of sodium chloride are added. The contents are well mixed and the spectrophotometer is set to read 100-percent transmission at 575 millimicrons with this solution. Three drops of a 10-percent solution of sodium hydroxide are then added to the same tube and it is inverted and read on the spectrophotometer. The transmission percentage is noted and the percentage of dye retention is obtained from the curve plotted from a standard bromsulfalein solution, following the conditions of the test wherein 10 mg. per 100 ml. is considered 100-percent retention.
Comment
The standard procedure for the determination of dye retention using the Hynson, Westcott & Dunning Comparator Block was abandoned because various degrees of hemolysis in the samples would result in readings that indicated as much as 5-percent retention when no bromsulfalein was present. Low retention figures, therefore, could not be expressed with any degree of certainty, as results were often not reproducible to within ±5-percentretention. Furthermore the method was time-consuming.
The test was set up on the Coleman Junior Spectrophotometer Model No.6, using a 1:6 dilution of plasma and reading the color of the alkalinized bromsulfalein at 575 millimicrons.
Renal Function Tests
Determination of Mannitol-Modified from Smith, H.24
MEASUREMENT OF GLOMERULAR FILTRATION RATE
Reagents
1. A 20-percent yeast suspension. (Bakers` yeast, 25 Gm., is placed in about 100 ml. of water, allowed to incubate overnight, and then washed by repeated centrifugation until a clear supernatant is obtained(about 6 washings are necessary). The resulting suspension is diluted to contain 20 percent by volume of yeast. This is washed several times each day
24In GOLDRING, W., and CHASSIS, H. Hypertension and Hypertensive Disease. New York, The Commonwealth Fund, 1944. Appendix D.
347
before using and readjusted to the 20-percent volume.)
2. 1.1 N sodium hydroxide.
3. Zinc sulfate solution. (A solution of zinc sulfate is prepared and adjusted so that 6 ml. of zinc sulfate are equivalent to 2.2 ml. of 1.1 N sodium hydroxide.)
4. 0.005 N sodium thiosulfate. (The normality is determined by using 10 ml. of 0.010 N potassium iodate. The factor for 0.005 N thiosulfateis: 1 ml. = 4.6 mg. of mannitol. The factor for the determined normality is calculated daily rather than adjusting the strength of the thiosulfate.)
5. Potassium periodate, 0.1-percent solution. (Prepared with the aid of heat.)
6. Sulfuric acid, 5 percent by volume.
7. Acid potassium periodate. (A solution of three parts of 0.1-percent potassium periodate and two parts of 5-percent sulfuric acid is prepared daily.)
8. Potassium iodide, 50-percent solution. (Prepared just before the analysis is made.)
9. Starch, 1-percent solution. (Prepared just before the analysis is made.)
Procedure
Six ml. of the 20-percent yeast suspension are placed in each of as many tubes as there are specimens and in a blank tube.
For plasma analyses, 1 ml. of water is first added to each of the yeast tubes and then 1 ml. of each mannitol-containing plasma specimen is added. Similarly, to another yeast tube are added 1 ml. of water and 1 ml. of blank (mannitol-free) plasma.
For urine analyses, the urine samples are diluted to contain from 100 to 150 mg. of mannitol per 100 ml. of urine. Two ml. from each such diluted sample are added to 6 ml. of yeast. Another tube containing 2 ml. of water and 6 ml. of yeast serves as the urine blank.
The yeasted tubes are shaken at intervals, and allowed to stand for20 minutes, then centrifuged, and the supernatant fluid is decanted. Fourml. of each supernatant are measured into 6 ml. of zinc sulfate solution, mixed, and 2 ml. of 1.1 N sodium hydroxide are added. The tubes are shaken vigorously, and allowed to stand for 10 minutes, centrifuged, and filtered. Two ml. of each filtrate are placed in a 50-ml. Erlenmeyer flask, and exactly5 ml. of acid potassium periodate are added with scrupulous care with an Ostwald pipet. A glass bead is placed in the flask and a glass stopper is placed in the mouth of the flask to effect condensation. The contents are boiled gently for 5 minutes and when cooled 1 ml. of 50-percent potassium iodide is added. The liberated iodine is titrated with sodium thiosulfate, adding 0.5 ml. of starch just before the endpoint and titrating until the blue color disappears.
348
Calculation
Plasma
ml. of thiosulfate used for plasma blank - ml. of thiosulfate for sample= ml. of thiosulfate for mannitol in plasma.
mg. of mannitol per 100 ml. of plasma = ml. of thiosulfate used x 4.6(thiosulfate factor) x 24 (dilution factor).
Urine
ml. of thiosulfate for water blank - ml. of thiosulfate used for urine sample = ml. of thiosulfate for mannitol in urine.
mg. of mannitol per 100 ml. of urine = ml. of thiosulfate used x 4.6x D x W x 12 (dilution factor).
Where:
4.6 = thiosulfate factor
D = urine dilution
W = washout dilution factor
12 = dilution factor for analysis
Mannitol Clearance (rate of glomerular filtration):
Cm (in ml./minute = V x Um/Pm
Where:
Cm = mannitol clearance
V = urine volume in ml. per minute
Um = mg. mannitol in 1 ml. of urine
Pm = mg. mannitol in 1 ml. of plasma
Para-Amino Hippuric Acid
MEASUREMENT OF EFFECTIVE RENAL PLASMA FLOW
AND MAXIMUM TUBULAR EXCRETORY CAPACITY
The method of Homer Smith25 was followed.
Phenolsulfonphthale in Test-Modified-AnalyticalProcedure26
Reagents
1. Sodium hydroxide, 2-percent solution.
25Ibid.
26In TODD, J. C., and SANFORD, A. H.: Clinical Diagnosis by Laboratory Methods. 10th ed. Philadelphia, W. B. Saunders, 1943, p. 163-167.
349
2. Acetic acid, 10-percent solution.
A standard curve is prepared from the phenolsulfonphthale in standard solution according to conditions of the test, blanking out with the acid color of the indicator at 540 millimicrons.
Procedure
The volumes of four urine specimens (timed) are measured and aliquots representing one-hundredth of the volume of each specimen are each pipeted into two cuvettes, one being designated as the acid tube and one the alkaline tube for the individual specimens. All the samples are diluted to 9.75 ml. with water, and to the alkaline tubes 0.25 ml. of the sodium hydroxide solution is added, and 0.25 ml. of the acetic acid to the acid tubes. Unless the solutions are absolutely clear, they are filtered. The alkaline tube is read in the spectrophotometer at 540 mµ, blanking out with the corresponding acid tube. The percentage transmission is noted for each alkaline tube and the milligrams of phenol sulfonphthalein content are recorded from the chart. In the event that excretion is markedly diminished, the procedure is repeated, using one-tenth aliquots of each specimen and dividing the chart readings by ten.
Comment
This method is much more accurate than methods depending on the usual comparator block because color due to urinary pigments is entirely blanked out.
Urinalyses
Routine Urinalysis
Specific Gravity.-Specific gravity is measured with a urinometer. If the specimen is not sufficient, the specific gravity is determined by weighing.
Appearance.-The color and appearance of the urine are noted.
Albumin.-Approximately 8 ml. of the specimen are placed in a test tube, the upper part of which is heated gently to the boiling point, any change in turbidity being carefully observed. Three drops of acetic acid in 20-percent solution are added and the upper portion is again heated to boiling. The heated portion is compared with the portion in the bottom of the tube, and depending upon the density of the precipitate, is read as negative, trace, 1-plus, 2-plus, 3-plus, or 4-plus.
350
pH.-Indicators used: Phenol red, bromcresol purple, and methyl red.
Procedure for determining hydrogen ion concentration: Three tubes of the same size as the indicator tubes are used, each of two of them containing 1 ml. of urine and 4 ml. of water, and the third containing 5 ml. of water only. To one of the tubes containing urine 0.25 ml. of bromcresol purple is added. The color resulting is compared with the standard solutions,27arranging the tubes so the diluted urine to which the indicator has been added is backed by distilled water and the standard tube is backed by the other diluted urine tube. If the pH is above 7.0, phenol red is used in a similar manner. If the pH is below 5.8, methyl red is used. Methyl red ranges from red to yellow between pH of 4.4 and 6.0.
The Benzidine Test.-Reagents: (1) Benzidine solution. (Five Gm. of a reagent grade of benzidine are dissolved in 50 ml. of glacial acetic acid with the aid of gentle heat, cooled, and diluted to 250 ml. with distilled water, 1 Gm. of animal charcoal is added, and the mixture is shaken and filtered into a brown bottle. It should be kept cool.) (2) Hydrogen peroxide,3-percent solution. (3) Hemoglobin standard, 20 mg. of hemoglobin per 100ml. in boric acid, 1-percent solution. (Lasts a week or 10 days.)
Procedure for performing the benzidine test: To 2 ml. of benzidine reagent in a clean tube are added 0.2 ml. of urine and 1 ml. of hydrogen peroxide. This is allowed to stand for from 30 to 60 minutes, the shorter time being for higher temperatures, and is then diluted to 10 ml. with 20-percentacetic acid solution. The red color may turn blue at this point, in which case the solution is allowed to stand in a warm place until the red color again develops. The standard is prepared exactly as if it were a sample. The solutions are filtered and compared in the colorimeter, with the unknown set on 20 millimeters. The reading of the standard yields the milligrams of hemoglobin per 100 ml. of urine.
Bile (Rosenbach`s Modification of Gmelin`s Test28).-A portion of the urine is filtered and a drop of fuming nitric acid is introduced into the cone of the filter paper. A succession of colors--green, blue, violet, and red in a ring pattern--is interpreted as a positive result.
The following urinalyses were performed by the standard methods indi-
27Preparation of the Clark and Lubs standard buffer mixture is described on p. 24 of HAWK, P. B., and BERGEIM, O. Practical Physiological Chemistry. 10th ed. Philadelphia, Blakiston, 1931.
28Ibid. Page 762.
351
cated: Ammonia (Folin and Bell29); urea nitrogen (Folin andYoungburg30); titratable acidity (Henderson and Palmer31);chlorides (Schales and Schales32).
Organic Acids in Urine-Modified from Van Slyke and Palmer33
Reagents
1. Calcium hydroxide.
2. Thymol blue indicator solution. (0.1 Gm. of thymolblue and 2.1 ml. of 0.1 N sodium hydroxide are made up to 100 milliliters.)
3. 0.50 N hydrochloric acid.
4. Phenolphthalein. (1 percent in 50-percent alcohol.)
Procedure
The urine is tested for albumin. If the albumin is 1-plus or higher, a noted volume of urine (greater than 100 ml.) is acidified with 0.5 ml. of concentrated hydrochloric acid, boiled for several minutes to coagulate the protein, cooled, made up to the initial volume, and filtered. If the urine is protein-free, it is used directly. Next, 0.5 ml. of phenolphthalein is added to 100 ml. of urine (or the protein-free urine filtrate) and powdered calcium hydroxide is added until the body of the solution turns pink (about2 to 4 Gm. are required). The mixture is allowed to stand for 1 hour. It is then filtered and 50 ml. of the filtrate are measured into a 125-ml.Erlenmeyer flask, decanting the remaining filtrate into an identical flask. To discharge the phenolphthalein color in both flasks 0.5 N HCl is added.
Two ml. of thymol blue are added to the 50-ml. sample of the urine, and 2 ml. of thymol blue and 0.3 ml. of 0.5 N hydrochloric acid to 50 ml. of distilled water, and the flasks are arranged for titration. (The 50-ml.urine flask is placed in front of a flask of distilled water, and the flask containing the dilute
29In HAWK, P. B., and BERGEIM, O. Practical Physiological Chemistry. 10th ed. Philadelphia, Blakiston, 1931, p. 829.
30Ibid. Page 825.
31In PETERS, J. P., and VAN SLYKE, D. D. Quantitative Clinical Chemistry. vol. II: Methods. Baltimore, Williams & Wilkins, 1932, p.827.
32In SIMMONS, J. S., and GENTZKOW, C. J. Laboratory Methods of the United States Army. Philadelphia, Lea & Febiger, 1944, p. 209.
33In PETERS, J. P., and VAN SLYKE, D. D. Quantitative Clinical Chemistry. vol. II: Methods. Baltimore, Williams & Wilkins, 1932, p.647-651.
352
hydrochloric acid and thymol blue is placed in front of the urine flask that does not contain thymol blue.) The 50-ml. urine specimen is titrated until its color matches the other set of flasks.
Calculation
[ (ml required - 0.3 x 24-hr. urine volume/100 ] - [Gm. creatinine in 24-hr. urine/100] = ml. of 1 N acid
Comment
The original method was modified by the use of thymol blue as the indicator instead of tropeol in oo, which was not available for the study, and by introducing into the comparator-block system a sample of the phosphate-free urine to compensate for urinary pigments in the titration flask.
Creatinine and Creatine in Urine-Modified from Folin and from Folin-Benedict and Myers34
Reagents
1. Saturated picric acid.
2. Sodium hydroxide, 10-percent solution.
3. 1 N hydrochloric acid.
4. 0.25 N sodium hydroxide.
5. Alkaline picrate. (Made by combining 5 volumes of saturated picric acid with 1 volume of 10-percent sodium hydroxide solution. It is freshly prepared before each series of analyses.)
Procedure for Determination of Creatinine
One-thousandth of the volume of a 24-hour urine specimen is made up to 10 milliliters. This is designated as the first tube. One milliliter of the contents of this tube is then diluted to 10 ml. with water, and designated as the second tube. Three ml. of the contents of the second tube are diluted to 10 milliliters, forming the third tube. Five ml. of the contents of this third tube are placed in a cuvette, and 2.5 ml. of alkaline picrate are added. The color is allowed to
34In HAWK, P. B., and BERGEIM, O. Practical Physiological Chemistry. 10th ed. Philadelphia, Blakiston, 1931, p. 835-837.
353
develop for 10 minutes and is then read in the spectrophotometer at500 mµ, blanking out with a solution containing 5 ml. of water and 2.5 ml. of alkaline picrate solution prepared at the same time as thesample. Grams of creatinine per 24-hour urine specimen are calculated by reference to the chart used for plasma creatinine and dividing by three.
Procedure for Determination of Creatine
To 2.5 ml. of the first creatinine tube, placed in a 25-ml. volumetric flask, is added 1 ml. of 1 N hydrochloric acid and the flask is placed in an autoclave at 120° C. for 15 minutes, cooled, and made up to volume with water. A portion of the contents of the flask is titrated with 0.25N sodium hydroxide, using phenolphthalein as an indicator to determine the amount required to neutralize 3 milliliters. A 3-ml. aliquot is neutralized and made up with water to 10 ml., 5.0 ml. are transferred to a cuvette,2.5 ml. of alkaline picrate are added, and the color is read as for creatinine.
The turbidity correction factor is determined and subtracted in this manner: The autoclaved solution in the volumetric flask is placed in acuvette, blanked out with the contents of the second creatinine tube, and its value in terms of optical density is determined. The value is multiplied by 0.3, changed to the transmission percentage at the creatine reading, and added to that reading.
Example:
Creatinine plus creatine reading: 50-percent T. (transmission)
OD of flask contents: 0.003
0.003 x 0.3 = 0.0009 = 0.001
OD of 0.001 corresponds to 1.5% T. at 50% T., making the corrected creatine reading 51.5-percent transmission.
The corrected creatine plus creatinine reading is converted to grams per 24-hour urine specimen by reference to the chart and then dividing by three.
The creatine content is determined by subtracting creatinine from the combined creatinine and creatine.
Comment
The method as modified had these advantages: (1) The analysis was setup on the spectrophotometer, which yielded more accurate colorimeter readings, and equipment and reagents were used sparingly, and (2) a turbidity correction factor was introduced into the creatine analysis which compensates for turbidity formed during the autoclaving process.
354
Determination of Myoglobin
Myoglobin, the red coloring matter of muscle, is a conjugated protein insisting of a protein part called globin and the iron pyrol compound known as hematin; it has a molecular weight of 17,000.
As stated in Chapter VIII, a spectroscope sufficiently sensitive to distinguish between hemoglobin and myoglobin was not available to us, and it did not prove possible to separate the two pigments in the plasma. The measurement of myoglobin in tissue and urine involved the following considerations:(1) It was necessary to find some property of myoglobin which would permit its quantitative separation from hemoglobin; (2) a convenient procedure for measuring the ultimately separated myoglobin, one that would be sufficiently sensitive to measure the small quantities anticipated in urine, was required, and (3) a rapid urine test was deemed essential since identification of myoglobin in the urine might influence the treatment of the patient.
Quantitative determination by means of the benzidine reagent was determined as the most satisfactory method. This test, however, was not satisfactory in media containing large amounts of phosphates and sulfates which caused gross precipitation of the benzidine reagent. These ions were present when it was attempted to separate myoglobin from hemoglobin by fractional crystallization procedures as described by Morgan35 and Rossi-Fanelli,36using lead acetate in 3 M phosphate buffer solutions or in concentrated ammonium sulfate. An efficient means of dialysis was not available at the time of the study and this method of separation was not pursued.
The myoglobin for further experimentation was extracted from perfused normal human skeletal muscle. A saline extract was made of finely minced muscle, eluting with constant shaking for 1 hour, using 2 ml. of saline for each gram of muscle tissue and allowing it to stand overnight in a refrigerator. The suspension was centrifuged to eliminate any red cells and then filtered (the muscle was completely bleached).
The concentration of myoglobin in this extract was determined by the benzidine test. The benzidine test measures the hematin part of the hemo-
35MORGAN, V. E.: The solubility of myoglobin in concentrated ammonium sulfate solutions. J. Biol. Chem. 112: 557-563,January 1936.
36ROSSI-FANELLI, A.: Crystalline human myoglobin; some physicochemical properties and chemical composition. Science 108: 15-16, July 2, 1948.
355
globin, or myoglobin molecule, and since the relationship of myoglobin(one hematin molecule, molecular weight 17,000) to hemoglobin (four hematin molecules, molecular weight 68,000) indicates the same proportion of benzidine-positive substance per unit weight of protein, reference can be made to standard hemoglobin solutions for quantitative measurement of myoglobin.
A portion of the stock myoglobin solution obtained as described above was diluted with normal urine to yield a level of 50 mg. per 100 ml., and a control solution containing 50 mg. of hemoglobin in 100 ml. of urine was prepared. On the addition of 0.5 ml. of 2.5 N sodium hydroxide to 10-ml.of each sample, a striking difference in the behavior of the two solutions was noted. The solution containing the myoglobin retained its reddish tint, while that containing the hemoglobin turned brown with the formation of alkali hematin. When acid, in equivalent amount to that of the alkali previously added, was added to each of the samples, the one containing myoglobin precipitated as a brownish-red protein, while in the hemoglobin tube the precipitation yielded a white protein material and the supernatant fluid remained brown due to the hematin. The contents of the tubes were then centrifuged.
The following chemical pattern indicates the different properties of the two proteins:
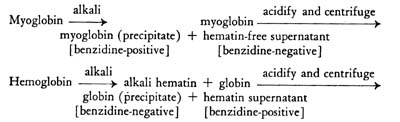
The supernatant fluid of the hemoglobin tube reflects the original concentration of the hemoglobin as hematin. The precipitate in the myoglobin tube was the myoglobin present. This dissolved readily in a little weak alkali and was made up to the 10-ml. volume. Quantitative estimation of myoglobin could then be made by the benzidine test.
Determinations made with hemoglobin solutions in urine indicated that on the average 90 percent of the hemoglobin could be recovered as hematin in the supernatant fluid while the precipitate would contain 10 percent of benzidine-positive material in the form of undecomposed hemoglobin. Determinations with myoglobin solutions in urine indicated that from 65to 85 percent could be recovered in the precipitate (the myoglobin fraction of the reac-
356
tion) and that the remainder had been decomposed by the alkali to alkalihemat in, yielding different proportions (15 to 35 percent) of myoglobin which would be measured as hemoglobin in the supernatant.
Recoveries from mixtures of myoglobin and hemoglobin indicated that separation could be effected between the two proteins, and that quantitative estimation of myoglobin in urine as well as in tissue was feasible. The following standards were established for interpretation of the findings:
1. A urine sample reflecting an analysis as 90 percent of the total benzidine-positive substance as hemoglobin and the remainder as myoglobin was considered to be all hemoglobin, while an analysis reflecting between 80 and 90 percent as hemoglobin was considered doubtful for myoglobin, and was also recorded as myoglobin-negative. A sample of urine yielding a level of less than 4 mg. of myoglobin per 100 ml., with a higher level in the hemoglobin fraction, was considered doubtful for myoglobin and recorded as negative.
2. A sample was considered to contain myoglobin beyond a doubt if it turned red or retained its reddish tint on addition of alkali and if, after separation of the protein, the precipitate was 20 percent or more of the total benzidine-positive substance. Recoveries in the myoglobin tube were considered as 70 percent; the value found was divided by 0.7 and the result reported in terms of the recovery factor.
For the first month of the survey each day`s run of benzidine-positive urines was accompanied by control recovery tubes of hemoglobin and myoglobin. Solutions of methemoglobin or hematin failed to show the analytical pattern described.
DETERMINATION OF MYOGLOBIN IN URINE
Following are the details of performing the test on urine.
Reagents
1. Benzidine solution. (As for plasma hemoglobin.)
2. Hydrogen peroxide, 3-percent solution. (As for plasma hemoglobin.)
3. Hemoglobin standard solution, 20 mg. per 100 cc. (As for plasma hemoglobin.)
4. Sodium hydroxide, 10-percent solution.
5. 2.5 N hydrochloric acid.
6. 0.1 N sodium hydroxide.
Procedure
To 10 ml. of urine in a test tube is added 0.5 ml. of the 10-percent sodium
357
hydroxide solution. (Reddening of the urine at this time serves as a qualitative test for the presence of myoglobin.) The solution is allowed to stand for 5 minutes, 0.5 ml. of the 2.5 N hydrochloric acid is added dropwise, mixing between each drop, and the solution is allowed to stand for 10 minutes, after which the tube is centrifuged for 10 minutes and the supernatant carefully decanted into another tube to be called the hemoglobin tube. To the residue in the first tube are added 9 ml. of water and 1 ml. of the 0.1 N sodium hydroxide, and this is mixed to effect complete solution of the protein precipitate. This is called the myoglobin tube. The "plasma hemoglobin" test is then made on the contents of both the hemoglobin and myoglobin tubes, using 0.2 ml. of each.
Calculation
mg. of hemoglobin per 100 ml. found in the hemoglobin tube x 11/10 =mg. of hemoglobin in 100 ml. of urine.
mg. of myoglobin per 100 ml. in the myoglobin tube divided by 0.7 =mg. of myoglobin per 100 ml. of urine.
If the urine contains over 100 mg. of benzidine-positive pigments per 100 ml., it is diluted to contain no more than from 50 to 75 mg.; the dilution is accounted for before making the final calculation. If the concentration in the myoglobin tube is low, instead of making the contents of this tube up to 10 ml., the precipitate is dissolved and made up to 2.5 ml. and the resulting calculation is divided by four.
DETERMINATION OF MYOGLOBIN IN TISSUE
The procedure followed for the determination of myoglobin in tissue is essentially the same as that for the determination of myoglobin in urine. The wet tissues are minced, finely ground, and weighed. Two ml. of saline are added for each gram of wet tissue and the mixture is shaken for 30 minutes and allowed to stand overnight. The contents of the tube are then centrifuged and filtered. Two ml. of the filtrate (corresponding to 1 Gm. of tissue) are placed in a tube, 8 ml. of water are added, and from this point the sample is handled as a urine sample.
Calculation
mg. of myoglobin per 100 ml. of diluted extract/0.7 x 10 = Gm. of myoglobinper Kg. of wet tissue.
![]()

